We at Cook Medical love to engage with customers and industry partners on social media. (You can find us all here.)

Dr. Richard Brady talks about #colorectalsurgery and Twitter at ASCRS.
Social media has already made a big impact for surgeons. To see it for yourself, take a look at the #colorectalsurgery hashtag. According to Mr Richard Brady, it has seen more than 3,400 users and 31,000 tweets in its first year. Or take a look at the #Ilooklikeasurgeon hashtag, which started in August 2015 and is still going strong. Tweets get especially fun during academic meetings and congresses. By using hashtags like #ACSCC16, #ACPGBI2017, and #ASCRS17, you can easily engage with fellow attendees or follow the event from home. These event hashtags seem to be growing. According to this tweet by Mr Sean Langenfeld, the #ASCRS17 hashtag was tweeted 6,723 times this year. In 2015, the #ASCRS15 hashtag was only tweeted 944 times.
During the recent tripartite meeting of the American Society of Colon and Rectal Surgeons (ASCRS), several surgeons spoke about their experience with social media.
Three social media strategies from this year’s ASCRS tripartite meeting
-
Share clinical data, said Mr Des Winter (@des_winter).
In his talk, Mr Winter explained how little we know about the world of science. Social media lets us connect with each other to share the bits of information we do understand. ‘Even when we have fantastic evidence, it doesn’t penetrate’, said Mr Winter. ‘It doesn’t penetrate because it has no influence. This is precisely what social media can do now. Social media can influence the way we think about the evidence that’s already there. It doesn’t change the content, but it gives you access to it.’
-
Manage your reputation, said Mr Sean Langenfeld (@seanlangenfeld).
On social media and on physician-rating sites, some surgeons occasionally see disgruntled posts. Mr Langenfeld suggests not responding on the digital platform. ‘You’re fuelling the fire. They’re looking for a response out of you’, said Mr Langenfeld. Instead, he suggested addressing patient concerns in person. He also suggested developing an online defense. ‘Provide as much positive information as possible between the online consumer and unregulated [physician-rating] websites.’
-
Take some breaks, said Mr Richard Brady (@researchactive).
Many surgeons experience information overload. Some feel pressured to stay connected at all times. This can lead to burnout. ‘Social media has great utility, but it’s addictive. We need to limit our use’, said Mr Brady. The brain reacts strongly to novelty, and each notification we see on social media boosts dopamine levels. ‘You need to train your brain to focus on tasks for a longer period of time without distraction.’ Mr Brady offered some tips. ‘Use shorter and less emails. Remove your phone from your bedroom at night. Don’t blindly scroll through your timelines.’
If you have any more thoughts on this, let us know. Tweet us at @CookSurgery.
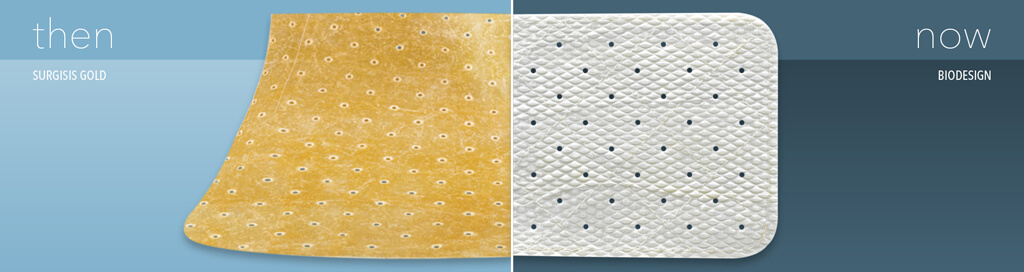
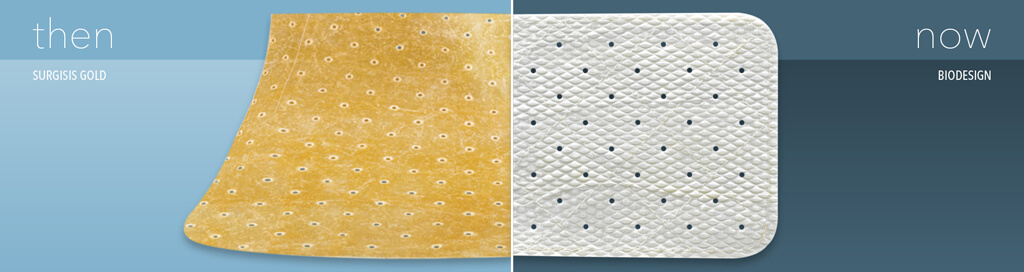
Biodesign® products from Cook Medical are constructed from small intestinal submucosa. But before our Biodesign products came into being, we had another line of small intestinal submucosa products. That product line was Surgisis®. In 2008, we created a new process for producing our small intestinal submucosa technology. Around that same time, we renamed the product line from Surgisis to Biodesign.
Our Biodesign product line for surgeons is similar to our Surgisis product line.
Why the changes?

Umesh, president of Cook
Biotech, listened to
surgeons’ suggestions.
When Cook Biotech first launched Surgisis products in 1998, they received positive feedback from surgeons. Umesh Patel, the president of Cook Biotech, remembers it clearly. Umesh was part of the team that first developed products from small intestinal submucosa. He and the Cook Biotech team worked hard to create Surgisis products, which were the first small intestinal submucosa products for surgeons.
‘We heard surgeons talking about how it could be improved’, says Umesh. ‘We’re always interested in improving our product.’ His team took a closer look at the product. They saw room for improvement in its handling characteristics and its biologic attributes. ‘We wanted to make a purer biomaterial. Lipids don’t have a place in the healing process. So, we reduced the amount of lipid in the material while maintaining other components that do have a place in the healing process.’
Then, they performed nonclinical studies. They saw more robust blood vessel ingrowth into the new material.1 They found that the new material rehydrated faster.1 In order to improve the operative performance, they included a quilting process.
‘We were satisfied once we saw the results of the clinical performance’, says Umesh. ‘We still continue to focus on improving our products and developing new ones.’
Learn more about small intestinal submucosa.
1 Data on file at Cook Biotech
 Vista® product-training courses are opportunities for surgeons to gather and discuss advanced techniques. Many courses for surgeons cover how to use Cook Medical products in component separation techniques for abdominal wall reconstruction.
Vista® product-training courses are opportunities for surgeons to gather and discuss advanced techniques. Many courses for surgeons cover how to use Cook Medical products in component separation techniques for abdominal wall reconstruction.
In a recent lab in the U.S., expert surgeons discussed when and why the transversus abdominis release (TAR) technique benefits patients. They facilitated a lab on TAR hernia repair.
We asked the expert surgeons a few questions.
Why is continued education so important?
Mr Sean Orenstein: Continued education allows physicians to explore skills and techniques that he or she may not be accustomed to, and/or reinforce and enhance skills already acquired. It’s easy to be in practice and continue to perform procedures in your comfort zone without pushing the envelope or trying something new. Learning new ideas and techniques allows surgeons to treat a wider variety of patient conditions, or help to examine their own limitations, thus paving the way for proper referrals to specialists.
What should a surgeon expect at a Cook Medical Vista event?
Mr JB Bittner: They should expect different things depending on the type of Vista. For basic, they should learn the basics of a disease process and techniques used to care for that disease process. For advanced, they should learn the steps of those techniques.
Mr Eric Johnson: Physicians should expect to have both a hands-on and didactic experience led by experts when they attend a Vista. They will have easy access to experienced surgeons that can answer questions and provide expertise.
- Mr Sean Orenstein is an assistant professor of surgery at Oregon Health and Science University.
- Mr JB Bittner is an assistant professor of surgery at the VCU School of Medicine.
- Mr Eric Johnson is a surgeon at MultiCare Colon and Rectal Surgery and the Tacoma General Hospital.
Mr Orenstein, Mr Bittner, and Mr Johnson are paid consultants of Cook Medical.
Take a look at upcoming Vista courses.
In 2012, a 43-year-old woman went into the operating theatre at QEII Hospital in Brisbane, Australia for an ordinary gynaecological procedure. While in recovery, she felt increasing pain. Soon she was in multiple organ failure.
Two surgeons, Mr Sanjeev Naidu and Mr Nai An Lai, shared how they saved her life and reconstructed her abdomen. “It’s been said that it’s one of our greatest saves,” said Mr Naidu.
“I don’t think we’re the best. I do not think we’re the most brilliant,” said Mr Lai. “But together we achieved much more than we could have achieved as individuals.”
4781158851001
brightcove
true
Note: This story reflects the experience of one individual. Every abdominal-wall-reconstruction case is unique. We at Cook can’t guarantee that every patient will experience the same level of success. Information included in this article should not be used as the basis for any treatment recommendation.
Mr Naidu and Mr Lai are not paid consultants for Cook Medical.


 Vista® product-training
Vista® product-training