6369357154112
brightcove
true
Synopsis
The European Aortic Data Collection (EADC) is a prospective, post-market, multi-centre observational study conducted across Europe.
The primary objective of the EADC is to collect patient-level data on Cook’s custom-made devices (CMDs), also known as patient-specific devices. This data helps assess the clinical safety and performance of endovascular treatments for complex aortic disease using Cook’s CMDs.
Since May 2023, the EADC has enrolled almost 800 patients across 18 sites with Prof. Stéphan Haulon serving as the principal investigator (PI).
In the video, Prof. Haulon discusses the study’s significance and the importance of collecting robust clinical data to evaluate product performance, drive innovation, and improve patient care.
Transcript
(0:10)
The European Aortic Data Collection: It’s a prospective, post-market, multi-centre observational study that we’re conducting across Europe.
(0:19)
The primary goal is to collect patient-level data on Cook custom-made device[s], otherwise known as a patient-specific device, also referred [to] as CMDs.
(0:29)
I am the PI of that study and [am] working with a group of physician[s] that have a high level of experience with complex aortic endografting.
(0:38)
This is from the arch… all the way down to the iliacs.
(0:44)
This helps to evaluate clinical safety and performance, the outcomes of endovascular treatment of complex aortic disease, using Cook CMDs.
(0:53)
We started the enrolment late May 2023, and we have already enrolled more than 500 patients. And 18 sites across Europe are enrolling, including Germany, UK, France, Italy, Sweden and Denmark.
(1:13)
Now we are—with those 500 patients we are now focusing on translating that data and planning publications.
(1:20)
What is nice is now that we have gathered over 500 patients’ dataset[s], we can start looking at the results and start sharing the initial EADC experience.
(1:32)
The importance of the collection of robust data for this type of procedures is vital.
(1:38)
Initiatives like this are critical for a few reasons.
(1:40)
So one, that data ensures that we understand how products perform in diverse patient populations and clinical settings.
(1:48)
And two, this data allows [us] to continue to focus on patient outcomes, refining and innovating treatment options with patients in mind.
(1:58)
Now this is where collaboration really shines between HCPs and Cook, as an innovative company, to ensure that we understand the data and translate it into best practices for patients.
(2:10)
Cook plays a vital role with EADC providing the resources and coordination needed to ensure that the study runs smoothly, because we need accurate data so that we can make the right decisions for our patients.
(2:23)
Something very special about EADC is how a small group of dedicated physicians are really focusing on making sure that the data is appropriate.
(2:32)
We will need this data to change our practice in the future or to support what we are currently doing.
(2:38)
So we want to make sure that we have the correct data to analyse.
(2:43)
So there’s a huge effort from Cook, HCPs, and us physician[s] to make sure that we are analysing the correct data and sharing it with the medical community.
Cook Medical welcomes you to the 2024 Charing Cross International Symposium.
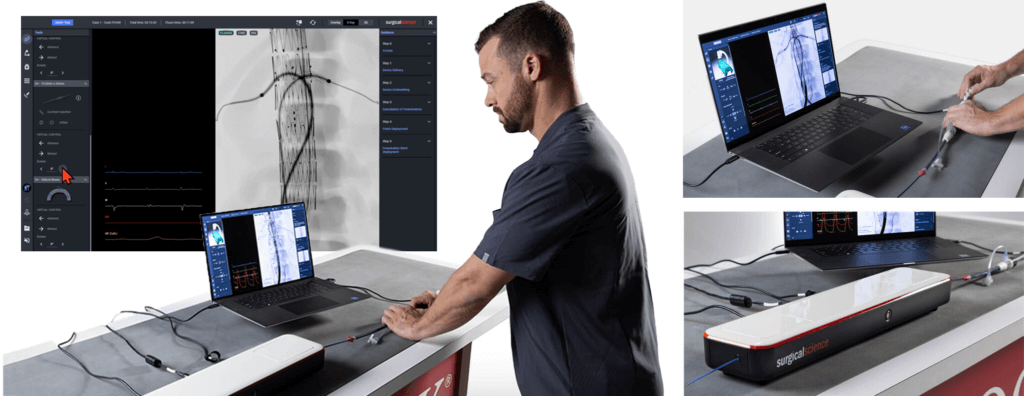
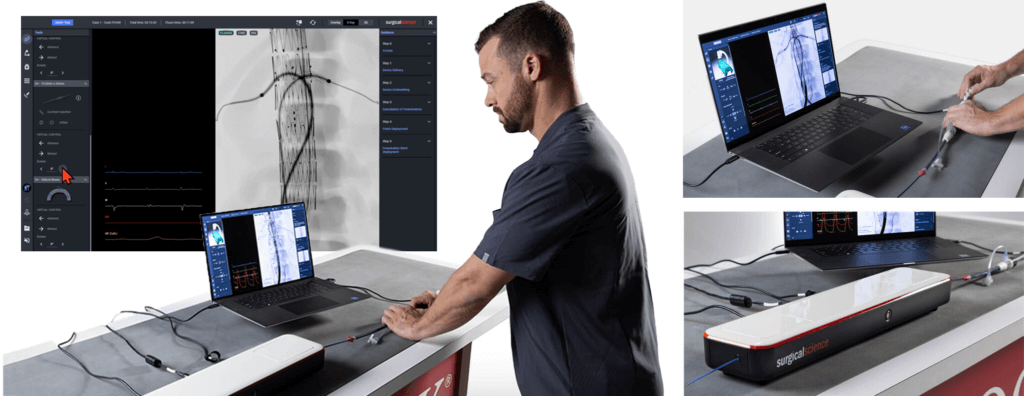
We invite you to stop by our booth in the exhibition hall to see and use the world’s first fenestrated simulator.
Enjoy a cup of coffee with us while challenging your cannulation skills.
Join our symposium
Tuesday, 23 April, 09:40–10:10, Theatre 2
Cook´s endovascular options to preserve the LSA
|
|
Introduction and moderation | Prof. Eric Verhoeven, Nuremberg, Germany
Preserve by fenestration | Prof. Nikolaos Tsilimparis, Munich, Germany
Preserve by branch | Prof. Tilo Kölbel, Hamburg, Germany
|
Wednesday, 24 April, 15:20–15:50, Theatre 1
t-Branch®: a versatile solution for TAAA repair with a proven track record
|
|
|
Introduction and moderation | Prof. Bijan Modarai, London, United Kingdom
t-Branch®: a versatile off the shelf endograft for TAAA | Prof. Nuno Dias, Malmö, Sweden
t-Branch®: a solution for TAAA with a proven track record | Dr Fiona Rohlffs, Regensburg, Germany
|
|

To learn more about our aortic program, devices, and services, visit here.
For news, product, and event information from Cook Medical, sign up here.
See you soon in London!

Cook Medical Training Unit – Training Suite 1 & 2
“Connect, train, and learn from the experts.”
The 23rd European Vascular Course (EVC) will take place in Maastricht, the Netherlands, from 10-12 March 2019. Cook Medical invites all EVC attendees to stop by the Cook Training Unit in the exhibition hall. Attendees will get the opportunity to connect, train, and learn from the experts in interactive and exclusive workshops.
To sign up for any of the workshops below, please contact Zoe Watson at zoe.watson@cookmedical.com.
Workshops EVC 2019
Aortic
Training Suite 1 & 2: Sunday, 10 March, 14:00-16:00
Challenges in the treatment of infrarenal aneurysms — considerations for a durable repair (EVAR): Key points when treating abdominal aneurysms
Learn about endovascular repair of abdominal aortic aneurysms and how to obtain a durable repair. Mr. Mark Tyrrell, Consultant Vascular Surgeon from London, has a large experience with EVAR and is ready to answer your questions in this interactive workshop. Using case presentations, Mr. Tyrrell will demonstrate the importance of planning for the best possible durable repair.
Training Suite 1 & 2: Monday, 11 March, 11:00-13:00
Strategies in the treatment of thoracic aneurysms – considerations for a durable repair (TEVAR)
Learn about endovascular repair of thoracic aortic aneurysms and how to obtain a durable repair. Professor Bijan Modarai, Consultant Vascular Surgeon from London, has a large experience with TEVAR and is ready to answer your questions in this interactive workshop. Using case presentations, Professor Modarai will demonstrate the importance of planning for the best possible durable repair.
Training Suite 1 & 2: Tuesday, 12 March, 11:00-13:00
Challenges in the treatment of infrarenal aneurysms – considerations for a durable repair in patients with a short neck (FEVAR)
Learn how to treat short necks using fenestrated EVAR. Dr. Nuno Dias from Sweden will share his experience with fenestrated grafts and how to obtain successful outcomes and the importance of planning for a durable repair.
Peripheral
Training Suite 1 & 2: Monday, 11 March, 14:00-16:00
Techniques in Lower Limb Preservation
“Approaches to below the knee angioplasty”
Speaker: Dr. Anton Collins, Interventional Radiologist, Belfast, UK
Discover how the changing approaches to below the knee angioplasty are contributing to the growing success of lower limb preservation, and hear from our experts about their techniques, technologies, and challenges. Learn how their tools of the trade and wealth of experience help to overcome these challenges to restore adequate perfusion to lower limbs using an endovascular approach.
“Vascular Limb Salvage Clinics: Are they supported by evidence of benefit?”
Speaker: Dr. Robert Davies, Vascular Surgeon, Leicester, UK
Participate in an informative and stimulating case study discussion, and learn from experts in the Vascular Limb Salvage (VaLS) clinic about their mission to quickly identify and treat patients with circulatory problems to effectively prevent amputation. This workshop will be very interactive, so we encourage you to ask questions to get the most valuable educational experience possible, and challenge our experts to gain a greater understanding of the thought processes behind the decision making for below the knee revascularization.
Venous
Training Suite 1 & 2: Tuesday, 12 March, 08:30-10:30
Venous interventions – Opening deep veins, PE prevention, and pelvic venous embolization
Speaker: Dr. Carsten Arnoldussen, Interventional Radiologist, Maastricht/Venlo
The attention for venous interventions has rapidly increased in recent years. Dr. Carsten Arnoldussen, a well-known venous expert, will discuss the appropriate indications and treatment techniques for patients with a deep venous obstruction. Dr. Arnoldussen will also explain IVC filter placement and retrieval as well as how to perform a pelvic embolization. Participants are encouraged to ask questions. After the initial presentation, participants will get hands-on experience at each workstation using the devices indicated for these treatments.
Workstation schedule:
- Workstation 1: Attendees will have the opportunity to perform venous stent placement. Helpful technical and procedural details for venous stenting will be discussed.
- Workstation 2: Attendees will perform an ovarian vein embolization and learn about the different techniques of coil placement.
- Workstation 3: Attendees will perform vena cava filter placement and retrieval. The indications for filter placement and the importance of retrieval will be discussed.
All physicians listed are paid consultants of Cook Medical.
AI-D47452-EN
 Mathew Wooster, MD, is in his fifth and final year of the integrated residency program at the University of South Florida in Tampa. Dr. Wooster shares his experience with FEVAR as a fellow and how it has impacted his job search.
Mathew Wooster, MD, is in his fifth and final year of the integrated residency program at the University of South Florida in Tampa. Dr. Wooster shares his experience with FEVAR as a fellow and how it has impacted his job search.
How did you get involved with fenestrated cases as a fellow?
Getting involved initially as a fellow is pretty straightforward. Basically, your attendings book a case and you figure out you have to learn how to do it. I already had a basic understanding of the procedure from going to a bunch of different meetings, so I was very curious about it and talked to my faculty about it. And when we got it here, I just jumped at the first case they were doing to try to start being involved—double scrubbing because at that time I was a junior resident. And then as I got more senior, planning the cases and doing the cases independently with the attendings.
What would you tell other fellows to help them get more exposure and experience with FEVAR techniques?
I don’t know that there’s anything anybody can do to get more exposure other than having the cases be available to them. It’s really a matter of knowing that the technology is there and whenever you see a patient with an aneurysm, you have to assess them and decide, is this patient a candidate? And if they are, advocate for it.
As you get ready to go into practice, how has learning these skills impacted your decision on where to go?
It’s helped in the sense that I have a pre-formed understanding of what I want to do. I want to have a fair amount of aortic work in my practice and so I was looking for a facility where that would be supported and encouraged as well as a facility that was going to both support and encourage fenestrated repairs.
And in terms of finding the right fit, I found that. I’m going to be going into university practice. They have a fairly large aortic experience right now. They have one of the larger fenestrated experiences in the country. The person who was doing most of those happened to be leaving, so I’ll slide right in as another person to help fill that role.
Did FEVAR make you more marketable coming out of fellowship?
Definitely. It was definitely very much sought after to know that you had somebody coming in who could offer really any level of endovascular or open experience. Being able to have the full array of treatments is crucial. There’s a lot of practices that have predominately older surgeons still, and they’re looking to bring in somebody younger who can offer this to patients. There’s other practices that have some younger people who are doing it, and they just want help. The reality is that a fenestrated case is at least a two-physician case. You need two sets of hands in addition to a tech. There are some practices where they just need a second person who knows what they’re doing with this stuff to be able to technically accomplish it. So knowing that I had that ability definitely made me more marketable to people.
Get stories like these sent to your email.
Sign up for our quarterly email newsletter to receive physician stories, product news, training opportunities and more in your inbox.
Mathew Wooster, MD, is an independent physician with no financial ties to Cook Medical.